This year’s ‘Time to Talk’ Day takes place on Thursday 3 February 2022 and focusses on creating supportive communities by having conversations with friends, family, or colleagues about mental health.
Research conducted by Mind and Rethink Mental Illness, the masterminds behind Time to Talk Day has shown just how important open conversations are in supporting everyone’s mental wellbeing. Conversely, a Time Change survey showed that 60% of people with a mental health problem waited over a year before telling their closest family and friends about it.
These two studies highlight how important it is to have, and continue to have, conversations with friends, family, or colleagues about mental health. After all, and as I’ve written on numerous occasions, we all have mental health and our mental health is fluid, in the same way as our physical health is fluid.
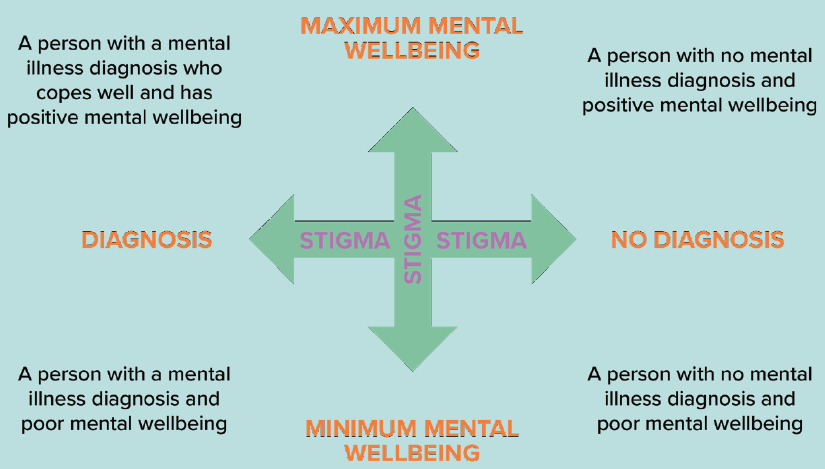
So here, I would like to delve a little deeper into what is referred to as the ‘mental health continuum’.
Historically, an individual’s mental health was viewed on a spectrum with good or positive mental health being at one end and poor mental health or mental ill-health being at the other end. A measure showing our mental health in one linear position.
However, this overly simplistic view doesn’t take into consideration that people can and do recover from mental ill health, or people who may have a diagnosed mental illness but who cope well with their illness.
A better, more fluid way of considering our mental health is by using this more holistic ‘continuum’ model.
It’s perfectly natural that some days we may feel good and be closer to the top of the vertical axis with maximum mental wellbeing or good mental health, and on other days we may not feel so great and be closer to the bottom. This is normal and that is what we mean by a fluid state, we are constantly moving up and down.
Interestingly, a 2011 report by the Centre for Disease Control and Prevention (more commonly known as CDC), estimated that only approximately 17% of U.S adults are believed to be in a state of optimal mental health. While directly comparable UK research is hard to come by, given that we lead very similar lives to those across the pond I would hazard a guess that our figures are not dis-similar.
It’s true that we will all spend time at different points on the vertical axis and that is just fine, in fact it would be unusual if someone felt exactly the same all of the time. However as we have explored previously, problems occur when we have poor mental health for a prolonged period or if it begins to interfere with our daily life. If either we notice this in ourselves or in others then this is absolutely the time to speak to someone about our how we are feeling and what we are perhaps feeling challenged by at this time.
Imagine you hurt your arm and you struggled to move it, you’d probably keep going for a week or so, maybe longer, hoping it would fix itself. However, if your arm didn’t get better and the movement got worse or stopped you working or doing things what you enjoyed, after a while you’d probably go and see you doctor or pop to the hospital for an X-Ray. Thus, beginning your recovery journey.
The same is crucial for people who may be finding everyday life a little tougher than usual and what’s more, just like a physical health condition, early diagnosis of mental ill health will help aid both recovery and the speed of recovery.
Unfortunately, one major factor why people don’t seek help if they are struggling with their mental health is due to the stigma that is STILL associated with it.
Thankfully this is changing but we still have a long way to go and talking about mental health helps to continually reduce that stigma, helping to create those all-important supportive communities where we can talk openly and feel empowered to seek help when we need it.
There are those of us who have never really spoken freely before about our mental ill health and having this type of conversation can feel daunting. If this is you then you may be worried you will say the wrong thing, put your foot in it, share too much or even make matters worse. However, I can assure you, you won’t!
If you are the person who is the recipient of someone’s first mental health conversation, there are some simple things you can do to help them to feel better and more supported while opening up. Please remember this is not a script and there is no need to get bogged down with these, the important thing is that you are there and listening so they can have the conversation.
- Start the conversation
- Choose a time and place that feels natural
- Ask twice
- Give them your undivided attention
- Listen and don’t judge
- Keep questions open ended
- Keep the conversation going
I have many real-life examples of these types of conversation as I’m sure you do too. You do not have to be a health professional to help lift the weight for whatever is bringing people down. A problem shared is a problem halved after all.
So if you notice someone being a little quieter than usual, perhaps more agitated or impatient its worth just checking in and starting that conversation.
And of course having conversations with friends, family, or colleagues about mental health should not just happen on one or two national or international awareness days. They should be ongoing and part of everyday practice.
However, by using the additional promotion that awareness days, such as these create, we help to make people more comfortable about discussing their own and their community’s mental health – if you haven’t already, please take the opportunity and use the 3rd February 2022 to kick start conversations and create those all-important supportive communities.